Neuroscience4Youth (N4Y) held its first annual online research case competition on October 18th, 2025, giving participants of both high-school and undergraduate-level the opportunity to explore the field of behavioral neuroscience with the prompt:
“What are the challenges and opportunities for implementing non-invasive brain stimulation (NBS) therapies for Major Depressive Disorder (MDD) in low-resource communities?”
Participants were encouraged to use a combination of meta-analysis, and comprehensive literature review searches to come up with an original research poster based on the prompt, which were then judged by the N4Y panel of judges! The top scoring groups were then asked to present their work to the N4Y judges for the final score determination, with the top 3 scoring groups providing unique and innovative insights into NBS therapies for MDD that takes into account the socioeconomic barriers that come with NBS therapies.
N4Y is incredibly honored to have given everyone who participated in the research competition the opportunity to explore the field of behavioral neuroscience in a way that sheds light not only on the limitations in treatment availability for MDD, but ways in which these limitations can be overcome with innovation and creativity. We are also honored to have given the opportunity for students passionate in neuroscience to get involved in scientific research, and understand the importance and necessity of bench-to-bedside research that takes into account existing socioeconomic barriers in order to inform the future leaders in neuroscientific research and neuroscience-based healthcare.
1st Place Winner: Zenab Amir, Ng Yun Lin Megan, Kaiden Pak
Implementing Non-Invasive Brain Stimulation for Major Depressive Disorder: Challenges and Opportunities in Low-Resource Settings
Background and Approach: Major Depressive Disorder (MDD) is the second leading cause of years lived with disability worldwide, underscoring its substantial global public health impact. The burden is particularly severe in low- and middle-income countries (LMICs), where only one in 27 individuals receive minimally adequate treatment, compared to one in five in high-income regions. Conventional treatments remained constrained by high costs, invasive procedures and restricted accessibility. Non-invasive brain stimulation (NIBS) approaches, including transcranial Direct Current Stimulation (tDCS) and repetitive Transcranial Magnetic Stimulation (rTMS), offer cost-effective and scalable alternatives suitable for low-resource settings. MDD continues to threaten individuals’ well-being and strain the capacity of health systems in affected communities. Structural inequities and economic barriers within LMICs further restrict access to care, contributing to rising prevalence. Current approaches often remain ineffective in these settings because they rely on invasive, resource-intensive procedures that are difficult to scale and are further limited by persistent shortages of trained professionals.
Findings: This literature review identifies the principal challenges associated with scaling NIBS technologies in LMIC, such as device costs, maintenance demands, workforce shortages, infrastructure limitations, regulatory gaps and low awareness. Our research also highlights promising solutions, including pilot programs, tele-supervised use, pooled procurement or donation models, training and task-shifting to non-specialists.
Conclusion: Overall research indicates that NIBS, particularly tDCS, provides affordable and viable care for MDD within LMIC contexts. Therefore, we propose five priority directions for future research: (1) conducting long-term LMIC-based trials; (2)training non-specialists with tele-supervision; (3) developing low-cost durable devices; (4) establishing regulatory frameworks for home use; and (5) integrating NIBS into community-based mental health systems.
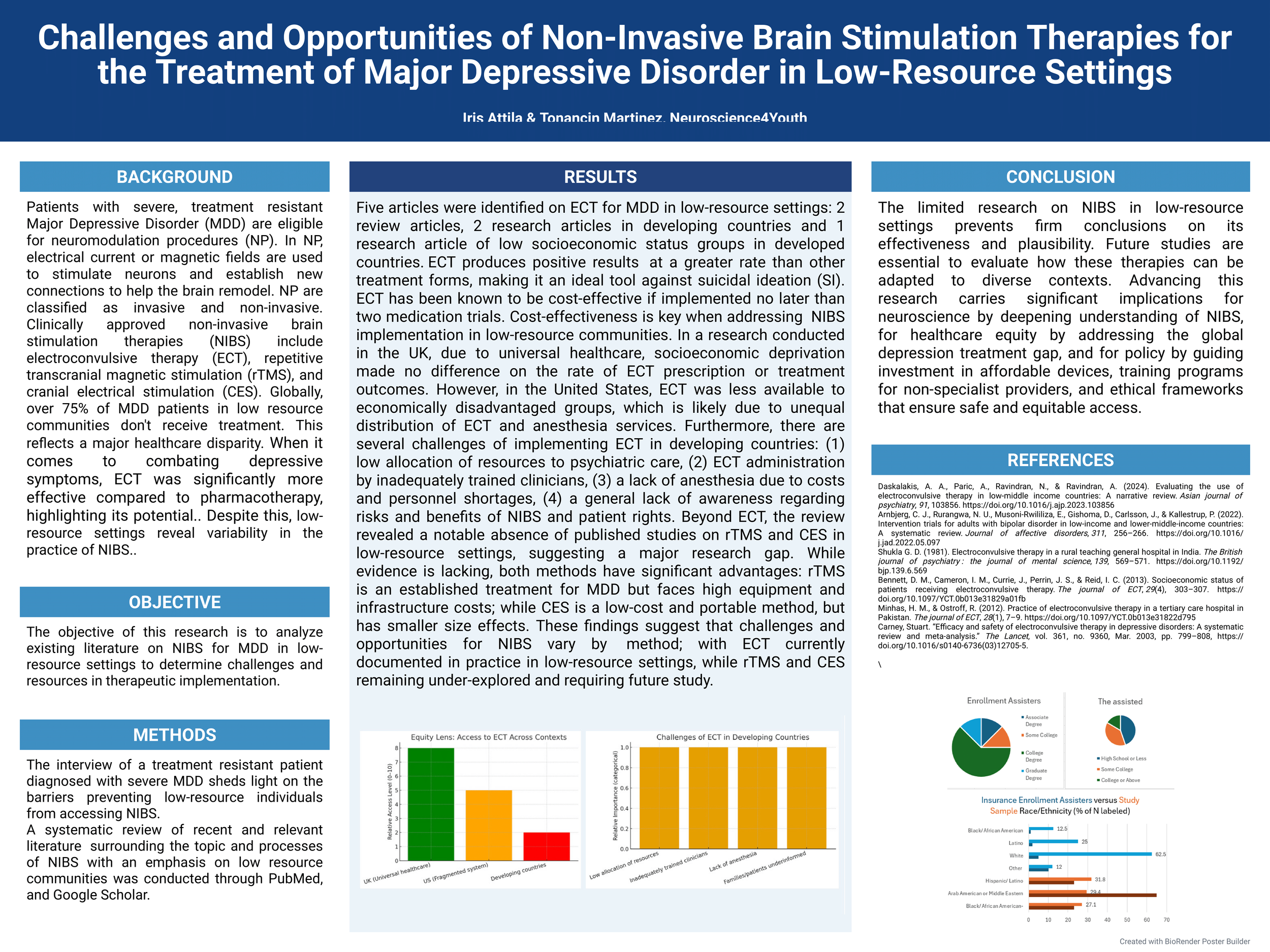
2nd Place Winner: Iris Attila, Tonancin Martinez
Challenges and Opportunities of Non-Invasive Brain Stimulation Therapies for the Treatment of Major Depressive Disorder in Low-Resource Settings
Background and Approach: Clinically approved non-invasive brain stimulation therapies (NIBS) for severe, treatment-resistant major Depressive Disorder (MDD) include electroconvulsive therapy (ECT), repetitive transcranial magnetic stimulation (rTMS) and cranial electrical stimulation (CES). The aim of this research was to analyze literature through PubMed/Google Scholar on NIBS for MDD in low resource communities (LRC) to determine the challenges and opportunities in implementation. Five articles were identified on ECT for MDD in LRC: Two review articles, two research articles in developing countries and one research article of LRC in a developed country.
Findings: In research conducted in the UK, due to universal healthcare, socioeconomic deprivation made no difference on ECT prescription or treatment outcomes. In the United States, ECT was less available to LRC. Furthermore, there are several challenges of implementing ECT in developing countries: (1) low allocation of resources to psychiatric care; (2) ECT administration by inadequately trained clinicians; (3) lack of anesthesia due to costs and personnel shortages; and (4) poor awareness of NIBS and patient rights. Beyond ECT, the review revealed an absence of published studies on rTMS and CES in LRC, suggesting a major research gap. Earlier ECT implementation reduces costs from ineffective pharmacotherapy while improving efficacy. Immediate reduction in symptom is crucial in combatting suicidal ideation. Evidence demonstrates consistent positive clinical response rates, with rare adverse reactions.
Conclusion: Challenges and opportunities for NIBS vary by method, with ECT currently documented in practice in LRC, while rTMS and CES remain under-explored and require future study. Recognizing both barriers and opportunities is essential for NIBS implementation.
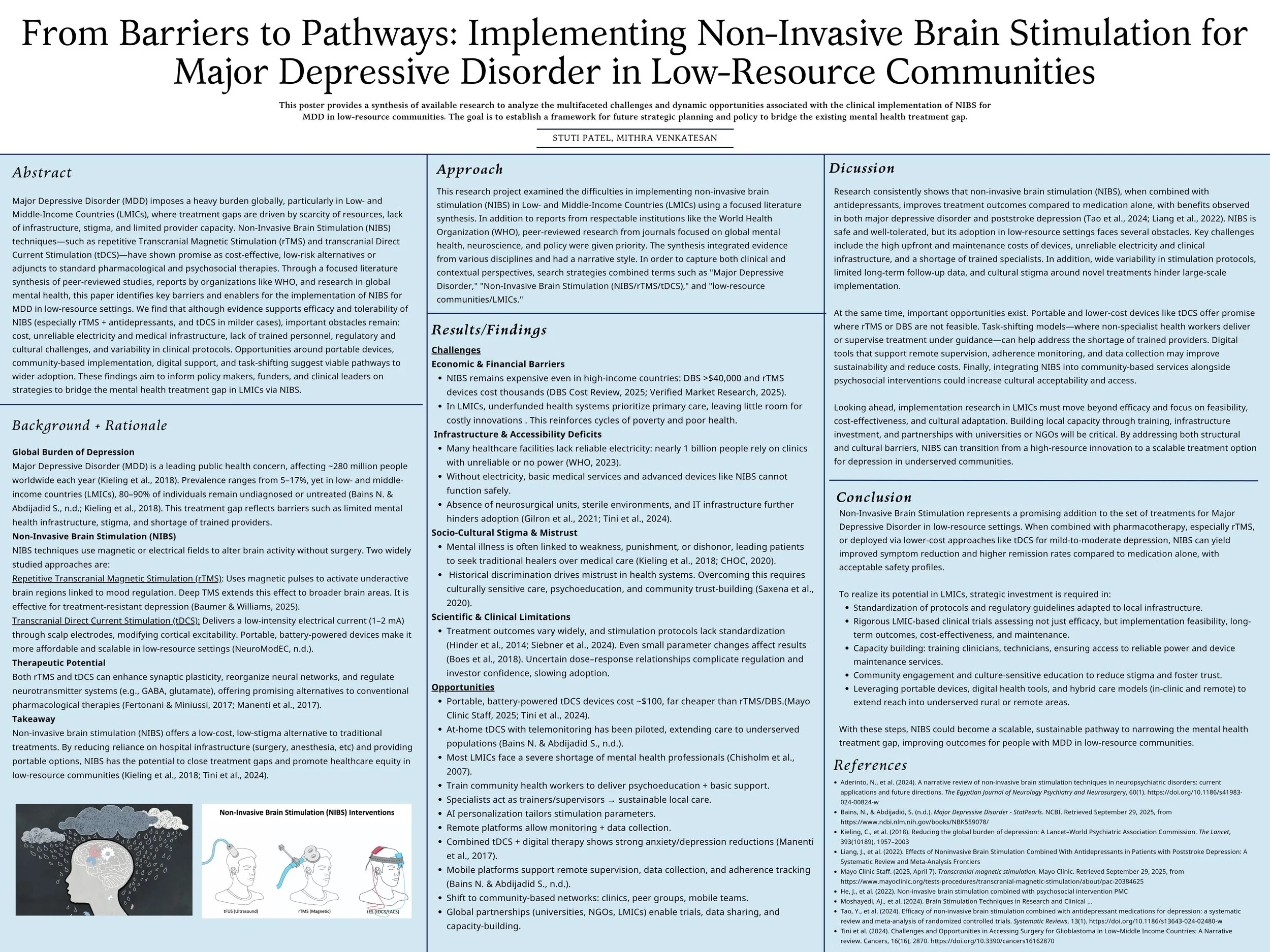
3rd Place Winner: Mithra Venkatesan, Stuti Patel
From Barriers to Pathways: Implementing Non-Invasive Brain Stimulation for Major Depressive Disorder in Low-Resource Communities
Background and Approach: Major Depressive Disorder (MDD) poses a global health issue, and the treatment gap is especially large in low-and middle-income countries (LMICs). Limited funding, shortages of trained mental health workers and a lack of reliable clinical infrastructure make it difficult for many people to access care. Non-Invasive Brain Stimulation (NIBS), including repetitive Transcranial Magnetic Stimulation (rTMS) and Transcranial Direct Current Stimulation (tDCS), shows promise as a safe and effective treatment option, either on its own or alongside antidepressants. However, its use in low-resource settings still faces limitations. This project looked at existing research to better understand the main barriers and possible strategies implementing NIBS in LMICs.
Findings: The main challenges identified were high device and maintenance costs, limited electricity and clinic space, a lack of trained staff and uncertainty around protocols and regulations. Cultural stigma and limited follow-up capacity can also affect consistent treatment. However, the research also pointed out the realistic opportunities. For example, portable and lower-cost tDCS devices, perhaps easier to introduce, and task-shifting models, where non-specialist health workers are trained to help deliver treatment, can increase access. Integrating NIBS into existing community mental health programs has also been shown to improve acceptability and support.
Conclusion: Overall, NIBS has strong potential to improve MDD treatment in low-resource settings, but successful implementation requires investments in training, protocol adaptation and community-based support models. With these strategies, NIBS could become an accessible and sustainable treatment option for depression in LMICs.