Interview by: Tina Zhou
Dr. Jason Samarasena is an interventional gastroenterologist at the University of California, Irvine (UCI) Medical Center’s Chao Comprehensive Digestive Disease Center. He specializes in the diagnosis and treatment of digestive diseases, including gastroesophageal reflux disease (GERD), pancreatitis, and biliary tract disorders through the use of state-of-the-art endoscopic technology. Dr. Samarasena has been recognized as the 2016 Teaching Attending of the Year by the UCI Gastroenterology Fellowship and has been recognized by Best Doctors in America for gastroenterology in 2015 and 2016. He has an outstanding reputation for patient satisfaction and is among the top five highest-rated doctors for patient satisfaction in the ambulatory surgery group. JYI had the pleasure of speaking with him about his profession.
JYI: Can you explain your field to someone who only knows the basics of science and medicine?
Gastroenterology is the study and treatment of the digestive system. Much of the diagnostic testing in this field involves endoscopy, which is the use of a camera to go into the digestive system to evaluate things with imaging, diagnose things with biopsy, or provide treatment with various interventions. Interventional gastroenterology is a practice that is almost completely procedural; these procedures usually involve gastrointestinal oncology, which means the evaluation and removal of pre-cancerous lesions in the digestive tract. We treat and remove lesions that are already cancerous and stage them based on their status along the progression of cancer. We use many endoscopic ultrasounds to better visualize the various digestive organs, and also biopsy tissue and provide therapy.
JYI: What does your work week look like?
Mondays are dedicated to administrative duties and research; Tuesday to Friday is all clinical care, which is taking care of patients. Thursday mornings I do clinical consults with patients. I also work weekends and evenings; being a physician does not mean you clock out at 5 or 6 pm. Physicians go home and complete charts at night, as well as writing and reviewing chapters and manuscripts and doing work on research projects. Every evening I put in at least 2 hours, sometimes more, on all of those things. On weekends, I put in about 4 to 5 hours doing work-related stuff because I have a very busy practice.
JYI: Do procedures usually go as you expect?
No. Procedures never happen as I expect; there are always surprises and challenges that come with performing procedures. It’s what makes working in this field exciting and interesting.
JYI: What are the biggest challenges of being a gastroenterologist?
I am involved in clinical, research, and administrative tasks, and also speaking engagements (once a month, sometimes industry-sponsored and can include grand rounds and lectures or evening talks). The biggest challenge I have is balancing clinical work with everything else, and then balancing family and life obligations with work. These are the biggest challenges for me as a teaching physician.
JYI: What are some things that you do that people would not typically expect to be a part of being a gastroenterologist?
Working with companies and vendors on trying out and developing new technology and products is something that comes with doing procedures that heavily involve state-of-the-art tools. I build connections with vendors and in doing so, I help improve the tools being used in practice and the techniques and methods with which to use them in procedures.
JYI: In what directions do you see your field growing or expanding towards, and how do you think it will impact healthcare in the (near) future?
There will be more technology to allow procedures that were once done surgically to now be done endoscopically. There will be more growth in pharmaceutical agents that we use for treating various diseases, and more of a focus on preventative health for cancer and other chronic diseases in this field. I also think that there will be additional incorporation of artificial intelligence in day-to-day documentation as well as computer-assisted detection of disease.
JYI: What are the active topics of research in your specialty?
Some of the active topics of research in gastroenterology include the use of artificial intelligence for detection and autonomous documentation. There is ongoing endoscopic device development, examples of which include cryotherapy technology for esophageal cancer, endoscopic early detection of pancreatic cancer, and endoscopic resection of cancer and other tumors.
JYI: How has research and technology changed your discipline over the past two decades?
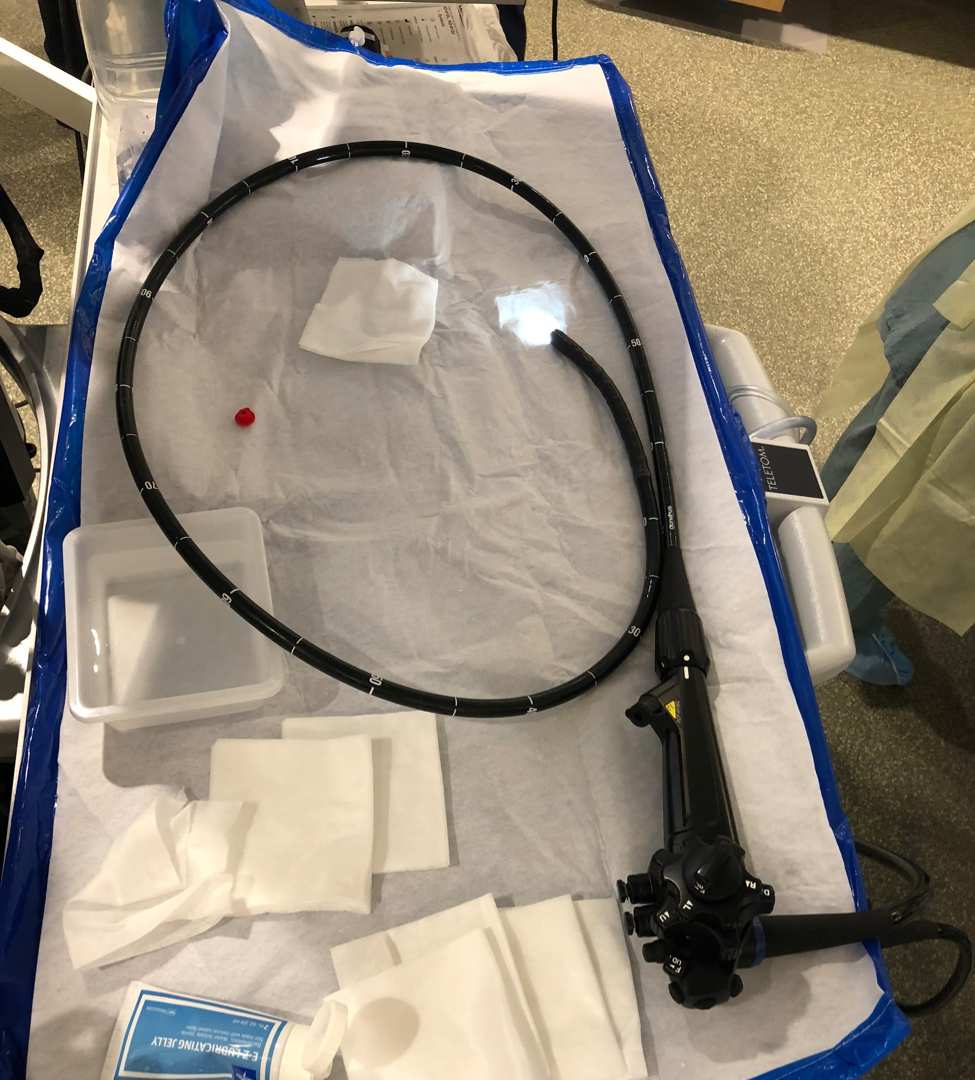
A colorectal endoscope after use in an endoscopic submucosal dissection (ESD), a procedure in which an endoscope is used to resect, or remove, a lesion or polyp from healthy digestive tissue. An endoscope can reach up to 6 inches deep into the duodenum, or the first section of the small intestine. Different tools can be inserted into the endoscope, one of which can be an ultrasound transducer. Using ultrasound, doctors can visualize any organ in the proximity of the esophagus, stomach, and intestines, including the liver, gallbladder, pancreas, adrenal glands, and kidneys.
My field is an extremely technology-based field, so technological development has had a huge, huge impact on the field. Cameras have become far more advanced, and scopes are safer, minimizing tissue injury. We have even developed microscopes that can fit through the channel of the scope. There are countless devices that can be put through the scope and countless more are undergoing research and development for therapeutic use. In the past decade, there has been a major shift as procedures that once needed to be done with surgery are now done with endoscopy, which is safer and better for patients.
JYI: What are the pros and cons of being a faculty member at an educational institution?
The pros are that I get to work with lots of doctors, and help train and mentor people at various stages of their medical careers. I am never the only one doing the procedure. Trainees, called fellows, enjoy the experience with me and provide a second eye and a second hand during procedures. Fellows also help me do my job more efficiently and help cut down my documentation time by over 50 percent. Academic institutions usually have the cutting-edge technology and people who are really interested in pushing the field forward and leading the charge in developing new equipment, devices, and ideas. Because I am never alone, I am constantly interacting with people. The biggest con to working at an academic institution is that it is a large entity, meaning that I do not have much control over big sweeping decisions being made that affect day-to-day work.